Need Prozac? Ativan? Ask your nurse practitioner; the landscape of non-physician prescribers is changing fast.

Certain areas of medicine are seeing a rapid influx in nurse practitioners and physician assistants, who are writing more prescriptions than ever before.
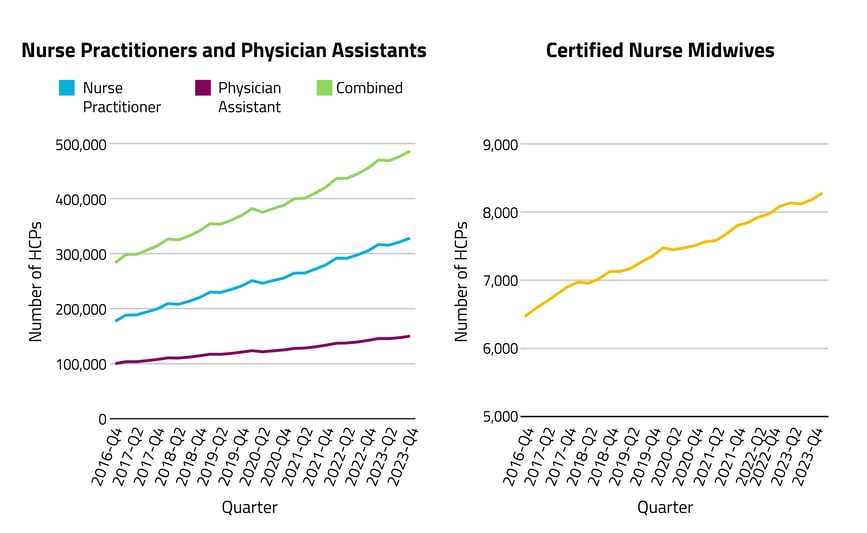
Healthcare delivery in the U.S. is undergoing a pivotal transformation due to the increase in telehealth and a strategic shift toward leveraging a broader array of healthcare providers to meet the nation's medical needs. An increasing number of nurse practitioners (NPs), physician assistants (PAs), and certified nurse midwives (CNMs) are now seeing patients across the healthcare continuum, and there are no signs of this trend slowing: Growth in employment for NPs and PAs is forecasted to reach 45% and 31%, respectively, by 2030.
More states now grant full practice authority to these types of providers, eliminating the requirement for physician oversight or collaboration. This broader prescribing authority, alongside the notable increase in telehealth services and non-physician healthcare providers, is particularly evident in certain specialties: family medicine, mental health, and women's health. The effects of this change are significant, influencing patient outcomes and the cost and availability of care, especially in underserved communities. However, this greater reliance on non-physician providers has sparked debate, particularly about patient safety, care quality, and whether this shift truly improves access to care in underserved areas.
In an effort to elucidate recent trends in the roles of NPs, PAs, and CNMs as part of the overall healthcare landscape as well as in specific areas of practice, Komodo looked at providers in active practice between Q4 2016 through Q4 2024. (These professionals do not represent a comprehensive list of non-physician prescribing providers, but they make up the majority and include the fastest-growing provider groups.) Our analysis was produced using our MapLab™ solution, which rapidly generates high-value insights and leverages out-of-the-box, healthcare-specific analytics on a unified platform. Several MapLab templates were used, including the Cohort Report to generate provider and prescription counts by drug group and patient insurance type.
Here’s what we found:
Over the past seven years, the number of non-physicians who can prescribe medication increased by 71%.
Between late 2016 and late 2023, the number of practicing NPs increased by 85%, PAs increased by 50%, and CNMs increased by 28%.
The number of prescriptions written — by all provider types — increased by 52% over the past seven years.
The increasing number of prescriptions that Americans are receiving is one piece of a growing systemic burden that, in light of physician shortages, have profound implications for healthcare access and quality, particularly in underserved communities, and is prompting calls for expanded roles and utilization of other healthcare professionals.
Non-physicians now write more than 1 in 4 of all healthcare prescriptions.
Non-physicians wrote about 17% of all healthcare prescriptions in 2016; by late 2023, that number had increased to 27%. This has largely been due to the increase in NPs, who now write 19% of all healthcare prescriptions, up from 10% in 2016, and prescriptions written by PAs rose from 6% to 8%. In this same time period, the overall number of drug prescriptions increased by just over half, while prescriptions written by NPs, PAs, and CNMs more than doubled, increasing by 144%.
More than 1 in 3 prescriptions for top psychiatric drugs* and contraceptives** are now written by non-physicians.
The biggest change seen throughout this analysis was in the share of prescriptions written by non-physicians for top psychiatric drugs (antidepressants and antianxiety and ADHD medications). Non-physicians wrote 16% of these prescriptions in 2016, a number that more than doubled to 34% by late 2023. Mental health also saw the greatest increase — 77% — in the number of non-physician prescribing providers. This could reflect greater need and/or demand for these medications overall. But it also demonstrates significant changes in systemic healthcare provision: While the total number of prescriptions written for psychiatric drugs increased by 44% during our time frame, those written by non-physicians increased by 205%.
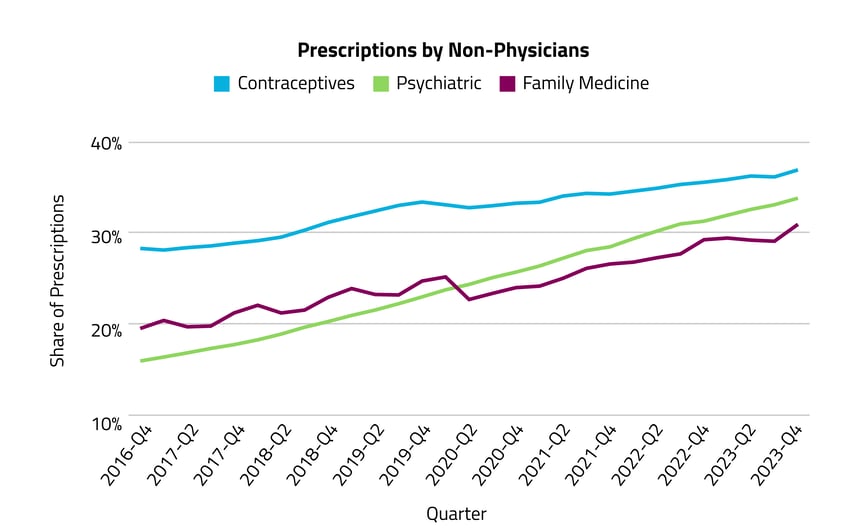
Family medicine and contraception also saw significant prescription-writing changes. Non-physicians prescribed 20% of common family medicine drugs*** in 2016, which increased to 31% in 2023. For contraceptives, it was 28% in 2016, increasing to 37% in 2023. Common family practice prescriptions and contraceptives had non-physician provider increases of 72% and 62%, respectively.
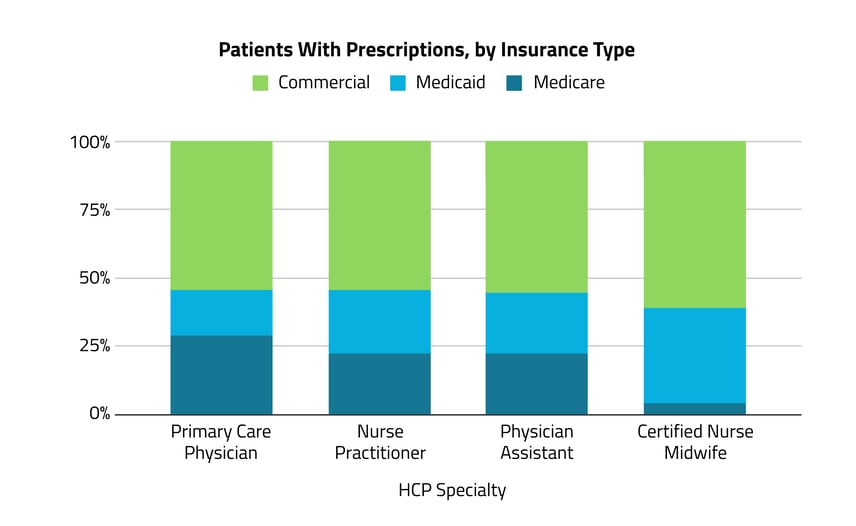
Primary care physicians and non-physicians treated a similar number of patients on both commercial and public health insurance.
Among patients who received a prescription from a non-physician, 55% were commercially insured and 45% were on Medicare or Medicaid. This was nearly identical to patients who received a prescription from a physician (limited to those in internal medicine, family medicine, and gender practice physicians), 54% of whom were commercially insured and 46% of whom were on Medicaid or Medicare. This overall similarity is surprising, although differences would more likely be seen among the most common prescriptions or among rural or underserved areas where there may be a higher likelihood of physician shortages. The only notable difference was among CNMs, where a larger proportion of patients who received a prescription were commercially insured (61%).
The U.S. currently faces a significant physician shortage that is projected to grow in the coming years: the Association of American Medical Colleges estimates a shortage of up to 86,000 physicians by 2036. This is felt across both primary and specialty care and is exacerbated by factors such as the aging population, the growing demand for healthcare services, and the high number of physicians reaching retirement age. The American Medical Association emphasizes the importance of taking immediate action to address this issue, considering the long lead time required to educate and train new physicians.
The impacts of any fast-paced changes in healthcare delivery should be closely monitored and tracked. Our analysis provides a comprehensive overview of the current state of this significant trend to inform the ongoing discourse on how best to structure and deliver effective healthcare in an ever-evolving landscape.
Addressing the physician shortage requires a multifaceted approach that focuses on both increasing the number of trained physicians and optimizing the entire healthcare workforce. This includes leveraging the full scope of practice of non-physician providers and embracing innovative healthcare delivery models such as telehealth. By doing so, the healthcare system can improve access to care, manage the increasing demand for healthcare services, and ensure high-quality care amid the challenges posed by the physician shortage.
*Psychiatric drugs include: antidepressants escitalopram and sertraline, benzodiazepines alprazolam and lorazepam, C-II stimulants amphetamine-dextroamphetamine and methylphenidate, and non-stimulant ADHD drugs atomoxetine, buprenorphine MOUD, and guanfacine ER.
**Contraceptives include: cervical caps, copper IUDs, diaphragms, female condoms, hormonal IUDs and implants, hormone-containing vaginal rings and patches, lacrimal duct implants (both temporary and permanent), injectables, intratubal occlusion devices, levonorgestrel implant systems, and spermicides.
***Family medicine drugs include: albuterol, amlodipine, amoxicillin, azithromycin, benzonatate, cyclobenzaprine, gabapentin, levothyroxine, lisinopril, and prednisone.







