How Race and Ethnicity Insights Expose Blind Spots in the Real World

Disease discriminates. Whether through genetic predisposition, social or environmental factors, or structural and systemic inequities that create barriers to care, disease burden is not borne equally.
Evidence of this can be found in virtually every condition in every U.S. Zip code. For instance, in colorectal cancer, Black Americans have the lowest five-year survival rates of any racial group in the U.S. and are more frequently diagnosed after their cancer had already metastasized. Or chronic obstructive pulmonary disease (COPD), where Black patients have 39% more emergency room visits and 43% more hospital admissions compared with their White counterparts. These examples exemplify that patient healthcare journeys from different racial, ethnic and demographic groups are rarely ever the same.
Tapping Race and Ethnicity Insight to Measure Impact
Inequality in care is a complex issue that permeates all aspects of the health system, from broad-based health policies and access issues to individual provider-level patient engagement. One opportunity that can have an outsized impact – and change the status quo from within – is health economics and outcomes research (HEOR). Tasked with validating the clinical and economic viability of a new therapy, HEOR teams are the critical link between breakthrough drug discoveries and the individual patients who will benefit most from those interventions.
Until recently, however, it’s been difficult for HEOR teams to identify discrete populations in any kind of systematized, efficient manner that illuminates the nuances of health disparities. Legacy claims databases often include inaccurate or incomplete self-identified racial and ethnic categorization of patients, and manual outreach to key opinion leaders often skew the captured patient population based on the demographics of a handful of teaching hospitals in major cities.
A Patient-Centric Approach to HEOR
Self-identified demographic data is a critical tool for HEOR, one that allows teams to develop a truly comprehensive approach to comparative effectiveness and value demonstration across every detailed subset of the total addressable population.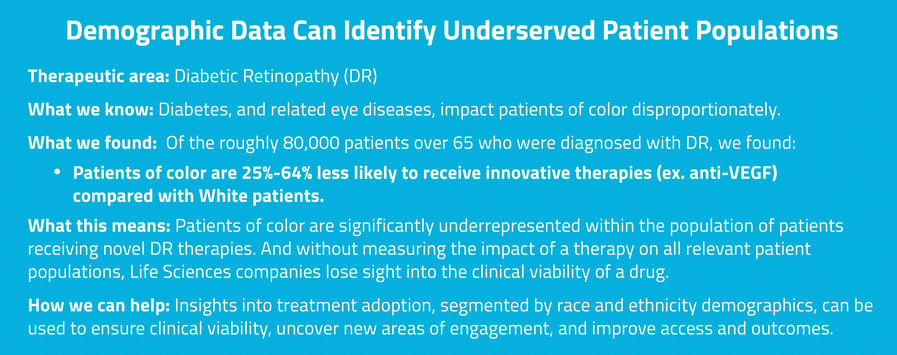 Expanding Access and Closing Gaps
Expanding Access and Closing Gaps
At Komodo Health™, we’ve made it possible for HEOR teams to look beyond structural limitations by expanding our Healthcare Map™ of de-identified real-world patient journeys to include hundreds of millions of race, ethnicity, and other demographic characteristics. Armed with this near-census level information, HEOR teams are now able to better model the clinical and financial impact of a new therapy across different racial and ethnic groups. From there, Life Sciences can better understand treatment efficacy, identify gaps in care, and improve provider engagement to specifically address health disparities.
The obstacles inherent to legacy datasets are a thing of the past; so are the excuses not to dig deeper, search further, and work harder to address bias and improve outcomes for patients in need. Access to nuanced patient journeys and demographic insights are here today. HEOR teams can now build their research strategies with a complete view of the real-world patient landscape to close the gaps in care that have created an unequal and unfair disease burden that has impacted so many, for so long.
Connect with us to learn more about how Komodo can unlock novel insights and use R&E data to power HEOR initiatives that are truly representative.
To see more articles like this, follow Komodo Health on Twitter, LinkedIn, or YouTube, and visit Insights on our website.





