Harnessing Better Data to Address Racial Disparities in Healthcare

Race, ethnicity, and socioeconomic factors continue to drive disparities throughout the U.S. healthcare system. From oncology to diabetes to sickle cell disease, too many communities continue to face obstacles that reduce their access to care, increase their time to treatment, and ultimately produce poor health outcomes.
To begin to address this problem, we first need to quantify the scope of it, identify at-risk segments of the population, and accurately target interventions that will have the largest impact. But that hasn’t happened. Instead, we’ve allowed systemic health system biases and inefficiencies to relegate these disparities in care to the long list of problems that are seen as either too complex or not profitable enough to prioritize.
Fragmented Data Perpetuates Racial Disparities in Care
That needs to change. The good news is that accessing the detailed data needed to comprehensively and cost-effectively cut through the noise and start the process of affecting real change is now possible. That was not the case for many years. Healthcare data has historically been siloed and difficult to access, with limited interoperability that prevented visibility into real-world patient journeys.
Because of this, each link in the chain, from primary care physician to the healthcare system to health plan to the life sciences industry misses a part of the patient experience. An institution might not see when the patient goes to a competing hospital, or when a patient moves out of state. An advocacy group misses patients that fit into their population and could benefit from their services. A payer doesn’t know when a patient pays out of pocket for a prescription because it’s cheaper than their insurance. Not understanding how an individual patient traverses the entire system over time creates a gap in care and prevents effective decisions for patients.
To show how this systemic fragmentation of data helps to perpetuate racial disparities in care, let’s look at sickle cell disease, a condition that disproportionately affects the Black community. Sickle cell disease is a genetic disorder in red blood cell formation. Mutation in this cell prevents oxygen from being carried effectively throughout the body and can cause damage to the heart, lungs, brain, and spleen. The average life expectancy for a patient with sickle cell disease is between 40 and 50 years. Each year, approximately 100,000 patients in the U.S. are diagnosed with sickle cell disease. Most notably, the vast majority of the 100,000 U.S. patients with the genetic disorder are African-American. All told, roughly 13% of African-Americans carry this gene.
The health care community has traditionally underinvested in this population. As a frame of reference, cystic fibrosis affects fewer than half the number of patients but receives 3.5 times the funding from the National Institutes of Health and 440 times the funding from national foundations.
In fact, despite the recent FDA approval of Adakveo and Oxbyrata—the first new therapies developed for sickle cell disease in the last 20 years—these three drugs reach fewer than one-quarter of adult patients who need treatment according to the American Society of Hematology.
The reasons for this wide gap in care can largely be traced to race-associated barriers to access and a lack of physician awareness, especially in community medical practice.
Tracking Complete Patient Journeys to Identify Gaps in Care
While creating new medications is an important step forward, patients need to receive that medication before it can help. To better understand what’s happening and where the system is breaking down, we looked at our Healthcare Map of real-world patient data to understand where sickle cell disease patients are interacting with our healthcare system.
Disease Burden of Sickle Cell Disease
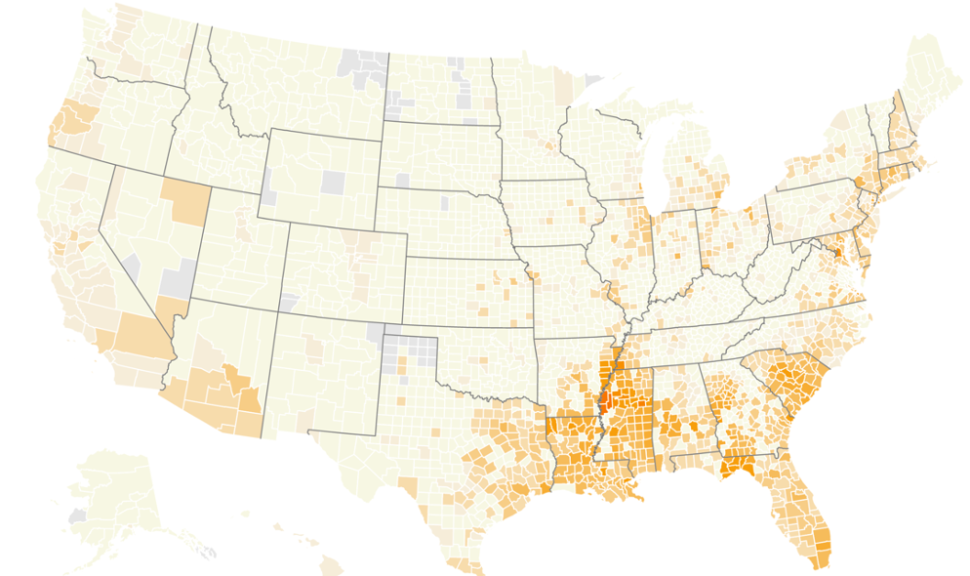
As the chart above indicates, the propensity of sickle cell disease is concentrated in the south. Drilling deeper we can see, for example, 64% of sickle cell disease patients were seen in the emergency department last year compared to about 44% of the general population, likely due to a complication of sickle cell disease. Furthermore, 64,000 sickle cell disease patients received blood transfusions in 2019. These are both signals of inconsistent treatment and poor disease management. Targeting this high-risk population with referrals to centers of excellence or specialists in sickle cell disease could result in better treatment and management, potentially avoiding emergency department visits and transfusions.
We are also able to identify exactly where those patients are treated, and then surface insights at the provider level and educate physicians (whether primary care physicians or hematologists) in order to get the best therapy to the patient or refer them to a center of excellence. This is important when you consider that a 2015 survey of 3,000 primary care physicians found that only 20% were comfortable treating sickle cell disease.
Affecting Change Through More Precise Targeting
The providers who are treating these patients need specialized education and resources that they are not currently receiving. But it is now possible to identify those providers in need and tailor clinical and scientific information to help them meet the needs of their populations. That level of granularity has never been possible before. However, it’s here now, and it’s exactly what’s needed to empower providers, population health officials, health plans, and the life sciences industry to zero in on disparities in care and address them immediately.
The data and tools for quickly getting to the ground truth of sickle cell disease burden are readily available with the insights needed to start the process of closing these gaps in care and ending racial disparities once and for all. It’s up to all of us to put that data to good use.
No one should have to live beneath the standard of care. As healthcare leaders, it is up to us to identify unmet needs and close the gaps.





