Finding the Signal in the Noise: Addressing the Data Challenges of Rare Disease

 Medicine in the 21st century has become almost algorithmic. For a broad range of common symptoms and routine conditions like diabetes, heart disease, or breast cancer, most people are quickly diagnosed and then ushered to the right providers for treatment. But that same streamlined efficiency that is so good at addressing common diseases often makes it harder to spot and treat rare disease.
Medicine in the 21st century has become almost algorithmic. For a broad range of common symptoms and routine conditions like diabetes, heart disease, or breast cancer, most people are quickly diagnosed and then ushered to the right providers for treatment. But that same streamlined efficiency that is so good at addressing common diseases often makes it harder to spot and treat rare disease.
Consider an example like hereditary transthyretin-mediated amyloidosis, or hATTR. This exceedingly rare genetic disease, which affects approximately 50,000 people worldwide, has more than 130 different genetic variations and manifests itself in a wide range of symptoms, including neuropathy, cardiomyopathy, and peripheral edema.
As a result of its complex genetic footprint, small patient base and association with such a varied range of common symptoms, the average hATTR case takes 10 to 15 years to diagnose and has a post-diagnosis survival rate of just 5 to10 years. In stark terms, that means that the average hATTR patient has 15 to 25 years to live, but spends two-thirds of that time searching for the source of the problem.
Countless examples like this exist throughout the healthcare system. Rare diseases like Gaucher disease, Hunter’s syndrome, Gorlin-Goritz syndrome, Li-Fraumeni syndrome, and many others tend to follow a similar pattern in which patients present with a range of symptoms that don’t fit neatly into a single box. As a result, they often end up bouncing from provider to provider, treating symptoms, racking up costs, and not addressing the real problem. The clinical impact, frustration, and financial strain create a significant burden for the patient that diminishes trust in our care system.
Using Real-World Data to Shake Up the Status Quo in Rare Disease Treatment
This is where predictive analytics and powerful, real-world patient databases have the power to redefine the way we diagnose and treat rare disease.
That’s precisely what we’re now starting to see happen with the treatment of hATTR.
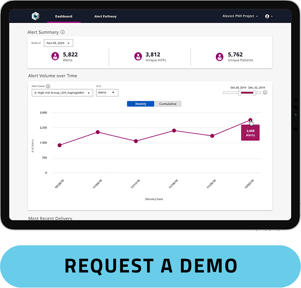
Using our Pulse predictive alert system, medical affairs teams have been able to pore over the complete healthcare journeys of the 320 million patients in our dataset to find signals consistent with a diagnosis of hATTR and make connections that might otherwise have been missed.
In fact, their early research into the disease has shown that there is a constellation of symptoms such as orthostatic intolerance, polyneuropathy, and ocular manifestations that may occur prior to diagnosis. Medical codes consistent with these conditions and associated symptoms are often predictive of a future hATTR diagnosis. In many cases, these specific symptoms are often present 36 months prior to a hATTR test, long before the disease starts to spiral out of control and finally results in referral to a specialist.
We’re seeing a similar phenomenon in research related to Gaucher disease. This genetic disorder, which is present at birth, affects just 1 out of every 40,000 live births globally and manifests itself as the buildup of fatty substances in the spleen, liver, and skeletal tissue. It can cause a wide variety of symptoms, including organ enlargement, fatigue, predisposition to fractures, and neuropathies. Though it is treatable, many patients go undiagnosed for years.
Using our Healthcare Map, we’ve been able to take entirely new approaches to spotting Gaucher earlier, through things like identifying trends in treatment, procedural, and diagnosis codes in patients known to have the disease. By identifying codes that occur frequently in this cohort, we can then look for undiagnosed patients who have similar patterns consistent with a future diagnosis.
In one early example from this work, we found that patients who received both abdominal imaging (ultrasound, MRI) and bone density testing within a 30-day window had a high likelihood of being screened for and diagnosed with Gaucher. Of 435 patients who underwent these imaging tests and then were subsequently diagnosed with Gaucher, 70% showed the pattern of these two imaging tests leading to specific genetic laboratory tests for Gaucher prior to diagnosis. Using these data, we are able to recommend Pulse predictive alerts at either the imaging or lab test event, which helps identify patients earlier than if we just relied on diagnosis.
Listening to the Signals
These types of signals are the critical missing links in the current system of healthcare. They allow us to identify patterns that can speed diagnosis and – importantly – they help the life sciences industry get vital treatments into the hands of those that need them most.
It’s a major achievement that medicine has advanced to a point where we can identify and treat common diseases so quickly. But we can’t stop there. We need to be able to apply the same level of streamlined, superefficient treatment to rare diseases that have perplexed healthcare providers for far too long. The signals are there. We need to start listening to them.





