Expanded Use of Telemedicine Exposes Stark Socioeconomic Disparity

Telemedicine is supposed to be the great equalizer. Celebrated for its potential to close disparity gaps in rural areas, praised for its ability to make specialists available to everyone and hailed as a critical lifeline during the COVID-19 pandemic, telemedicine has become an important component of the healthcare ecosystem. But, it’s not perfect. The surge in telehealth utilization during COVID-19 has revealed a number of troubling trends involving access to care that need to be addressed before the technology can reach its fullest potential.
We discussed one of these issues in a recent blog post, which highlighted distinct gaps in geographic utilization of telehealth during COVID-19. Ultimately, we found that some states – like Vermont and Rhode Island – had upwards of 44% of their providers offering care via telemedicine during the pandemic. Yet others – such as Missouri and Montana – had just 27% of providers offering these services.
Perhaps more troubling, though, we’ve also begun to see significant socioeconomic trends emerge in this data set.
Telemedicine Utilization Directly Linked to Income
Specifically, when we applied data on median income, derived from the American Community Survey, to our data set, we found that patient utilization of telemedicine – measured by billing claims we see in our Healthcare Map – has been directly correlated with income during COVID. All told, we found that providers in the 10% of U.S. counties with the highest median income were 47% more likely to bill for telemedicine than those in the bottom 10% of U.S. counties by median income level.
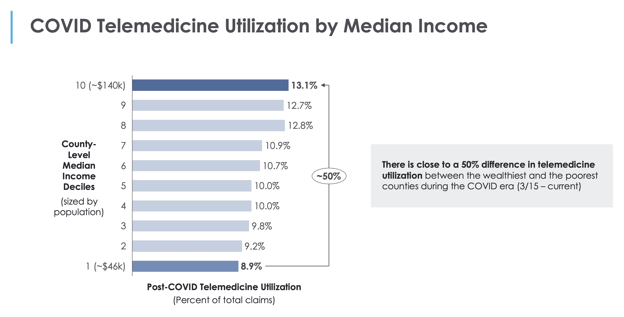
As the chart above indicates, the telemedicine utilization rate among those in counties with a median household income of $140,000 or more was 13.1% between March 15-May 15. By contrast, the utilization rate was just 8.9% among those in counties with a median household income of $46,000 or less. Across the household income scale, our analysis suggests that access to telemedicine was directly correlated to higher levels of household income.
Weighing the Public Health Impacts of Telemedicine
We’re not the only ones to spot this trend. Our partners at Kantar Health recently worked with us to explore this issue and published an analysis the Social Determinants of Telehealth in the U.S. using our Healthcare Map to find that the 3,000% surge in telehealth utilization during the pandemic was driven in large part by younger, wealthier patients. The findings reinforce the concerns raised by public health researchers from the Harvard T.H. Chan School of Public Health and Boston University School of Public Health who recently wrote in HealthAffairs that the nation’s community health centers – which serve more than 28 million low-income and disproportionately uninsured patients – have struggled to implement high-quality telehealth.
This first real test of telehealth at scale has exposed a digital divide phenomenon that researchers have been warning us about for many years. Some of the stats might be surprising for professionals who spend their lives developing healthcare technology, but they are important to acknowledge.
More than one in three US households headed by a person age 65 or older do not have a desktop or a laptop and more than half do not have a smartphone device. Children in low-income households are much less likely to have a computer at home than their wealthier classmates. And, more than 30 percent of Hispanic or black children do not have a computer at home, as compared to 14 percent of white children.
Countless variables like these affect access to care at a nationwide level. While our data shows that a growing portion of the U.S. has begun to embrace telehealth as a possible solution during the COVID-19 pandemic, it also illustrates some of the challenges that still exist in making this type of care available to everyone.
As of this writing, every state in the U.S. has implemented some form of executive order or temporary guidance on telehealth access, which govern Medicaid reimbursement for the service and heavily influence access, but they all vary widely and it is unclear how these policies will be maintained over the long term. It will be critical as healthcare policymakers, providers, payers and tech companies continue to experiment and innovate in this space that we all take into account the potential for unintended gaps in care, and continue to measure our progress along the way.





