COVID-19 and Mental Health in the Pan-Asian Community

Racism negatively impacts mental health. From children to elderly adults, studies have identified a host of negative effects that implicit and explicit systematic racism can have on communities of color.
Compounded by cultural, social, and socio-economic factors that may prevent individuals from seeking out care and resources, race-specific mental health challenges, although prevalent, often go undiagnosed and untreated.
A Spotlight on the Asian American Experience
This phenomenon has been felt acutely in the Asian American Pacific Islander (AAPI) community during the COVID-19 pandemic. In addition to the shared challenges associated with the pandemic itself, xenophobic and racist responses to COVID-19 spurred a wave of anti-AAPI hate crimes across the country. In fact, a survey conducted by Mental Health America in late 2019 (before the pandemic) found that 39% of AAPI respondents reported experiencing severe anxiety. In the first month after the coronavirus pandemic took hold in the United States, that proportion rose to 45%.
Despite these growing numbers, research by the National Latino and Asian American Study found that Asian Americans were significantly less likely to seek out mental health resources — while 18% of U.S. citizens overall sought mental health resources, only 8.6% of Asian Americans did so. A study by the University of Maryland identified many factors that may be contributing to this gap, including:
- Taboo around discussing mental health concerns in many Asian cultures
- Pressure to live up to the "model minority" stereotype — a view that inaccurately portrays Asian Americans as successfully assimilating into mainstream culture and having overcome the challenges of racial bias
- Discrimination due to racial or cultural background
In order to shed more light on the unique mental health experiences of the AAPI community, our Pan-Asian Heritage Dragons affinity group conducted an analysis using Komodo’s our Healthcare Map to track healthcare utilization for mental health support both before and during the COVID-19 pandemic. Comparing 2019 with 2021, we analyzed the patient journeys of Asian-identified patients (a group that includes Chinese, Indian, Japanese, Korean, and other Asian and Pacific Islander individuals) with at least one claim for depression, anxiety, bipolar, or schizophrenia.
Following are the highlights of what we found:
Asian Americans were three times more likely to be diagnosed with depression during the pandemic compared with White Americans. 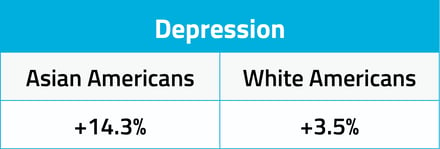 Compared to pre-pandemic levels, the proportion of Asian Americans diagnosed with depression increased by 14.3%, while White Americans only saw a 3.5% increase in diagnosis during that same time frame.
Compared to pre-pandemic levels, the proportion of Asian Americans diagnosed with depression increased by 14.3%, while White Americans only saw a 3.5% increase in diagnosis during that same time frame.
During the COVID-19 pandemic, anxiety diagnosis increased among Asian Americans while decreasing in White patient populations. 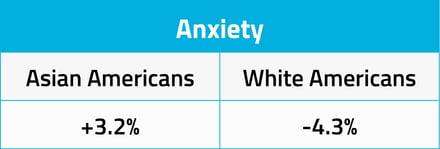 While White patients saw a decrease of 4.3% in anxiety diagnosis between 2019 and 2021, Asian American patients saw 3.2% increase — a difference of 7.5% —during the same period.
While White patients saw a decrease of 4.3% in anxiety diagnosis between 2019 and 2021, Asian American patients saw 3.2% increase — a difference of 7.5% —during the same period.
The increased rates of both depression and anxiety diagnoses among Asian American patients during the pandemic suggest a disparity in mental healthcare that has disproportionately affected a distinct racial demographic.
Trends in bipolar and schizophrenia diagnosis differed between Asian American and White populations. 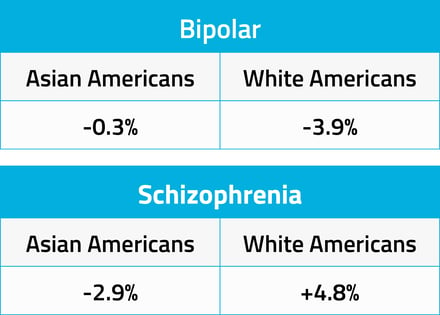 Bipolar diagnosis remained nearly the same for Asian American populations during COVID, with only a 0.3% decrease compared with pre-pandemic levels. However White patients saw a marked decrease in diagnosis, nearly 4%. White Americans had a significant increase in schizophrenia diagnosis as compared with Asian Americans, a difference of 7.7%.
Bipolar diagnosis remained nearly the same for Asian American populations during COVID, with only a 0.3% decrease compared with pre-pandemic levels. However White patients saw a marked decrease in diagnosis, nearly 4%. White Americans had a significant increase in schizophrenia diagnosis as compared with Asian Americans, a difference of 7.7%.
If similar trends for bipolar and schizophrenia diagnoses were seen across both Asian American and White populations, it could be attributed to the lower usage of healthcare systems overall during the pandemic. However, the increase in schizophrenia diagnosis in White patients — an increase of 4.8% compared with pre-pandemic rates — suggests otherwise.
The decrease in schizophrenia diagnosis among Asian Americans during COVID (-2.9%), may suggest an increase in undiagnosed cases. Additional analysis is necessary to investigate that hypothesis.
A Complex Challenge
The impact of the COVID-19 pandemic on Asian American communities is complex and deeply intertwined with cultural nuances, which aren’t always easily identifiable when assessing the healthcare system. However, this analysis can help to identify and elucidate pain points and inform solutions that can close gaps in care for patients of color and those who face health and care inequities. Komodo Health will continue to apply our race and ethnicity insights to identify opportunities for change in the healthcare system to reduce racial disparities in health and healthcare.
For more information about how Komodo Health can help to close gaps in care for minority populations, read our blog, 
To see more articles like this, follow Komodo Health on Twitter, LinkedIn, or YouTube, and visit Insights on our website.





